About the Medicare reforms
This guide was last updated in November 2024.
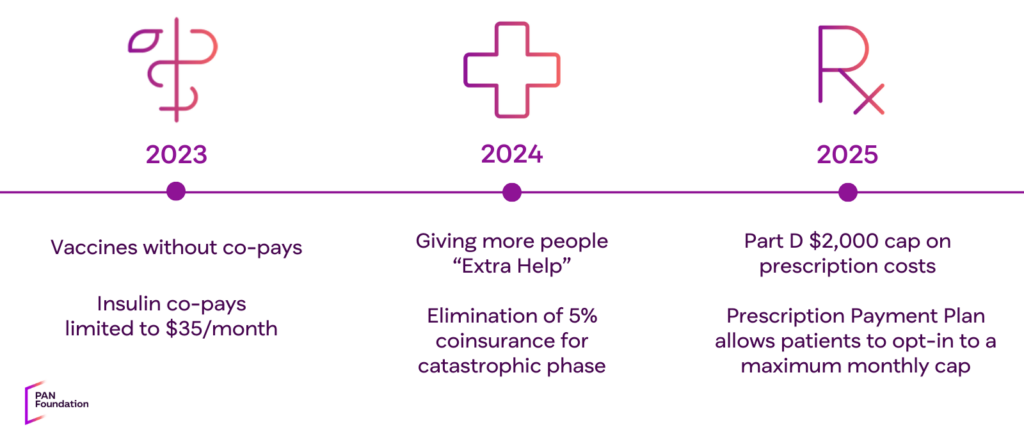
Six key reforms to the Medicare Part D program were passed in 2022 as part of the Inflation Reduction Act. Two changes went into effect in 2023, two in 2024, and the final two take effect January 1, 2025. Below, we describe the reforms and what people enrolled in Medicare Part D plans need to know.
The Medicare reforms apply to all standalone Medicare prescription Part D plans and Medicare Part C or Medicare Advantage plans that have prescription drug coverage. Medicare HMO plans are included if they offer drug coverage. The reforms do not apply to supplemental insurance, Medigap plans, or Red, White & Blue insurance, which covers Parts A and B of the Medicare program.
| Medicare reforms apply to | Medicare reforms DO NOT apply to |
| All Part D plans | Supplemental insurance |
| Medicare Part C (Medicare Advantage) plans. Most Medicare Advantage plans include drug coverage (Part D) | Medigap plans |
| Medicare HMO plans, if they offer prescription coverage | Red, White, and Blue insurance |
Bookmark our guides
If you or a loved one has Medicare Part D insurance, we encourage you to bookmark this webpage and our detailed guides below.
Download a guide presented by NCODA, in collaboration with the PAN Foundation, on Navigating Medicare with Confidence, which breaks down the Medicare changes for oncology healthcare professionals and patients.
You can also watch our explainer video and our educational webinar about the Medicare reforms.
Do the reforms impact my enrollment?
The Medicare reforms do not impact an individual’s current Medicare enrollment and should not impact decisions during open enrollment. During open enrollment, which runs from October 15 through December 7 each year, we encourage people to select plans that best match their current prescription and medical needs.
Which medication is best for you is a decision between you and your healthcare provider. During the open enrollment period, we recommend that you pay close attention to any changes in your current plan related to medications you may need and carefully review a potential new plan’s drug coverage, related copays, and related coinsurance.
What do the “parts” of Medicare mean?
Medicare is the health insurance program for people aged 65 or older in the United States. You may also qualify if you have permanent kidney failure or receive Disability benefits. Get familiar with what is covered by each “part” of the Medicare program to better understand this guide.
| PART A Hospital insurance | PART B Medical insurance |
| Inpatient hospital stays Care in a skilled nursing facility Hospice care Some health care Does not cover regular doctor visits or prescription drugs | Certain doctor’s services Outpatient care Lab tests Medical equipment Preventative services Ambulances |
| PART C Medicare Advantage, “all in one” alternative to Original Medicare | PART D Prescription coverage |
| Covers benefits included with Original Medicare Sometimes covers: dental, vision, over-the-counter items, etc. May include prescription drug benefits Most Medicare Advantage Plans (Part C) include drug coverage (Part D) | Prescription drugs Part D plans are offered by private companies approved by Medicare |
Medicare Part D cap of $2,000

Beginning January 1, 2025, people with Part D plans through traditional Medicare and Medicare Advantage plans with prescription drug coverage won’t pay more than $2,000 over the calendar year in out-of-pocket costs for their prescription medications. All prescription medications, including specialty medications, covered by Part D plans are included under this cap, including deductibles, copayments, and coinsurance for covered drugs.
It does not apply to costs for drugs that are not covered under a Part D plan, nor does it cover drugs covered under Medicare Part B, such as injectables and infused drugs.
The cap applies to all Medicare beneficiaries with Part D prescription drug coverage, regardless of income level. The new cap will help all people enrolled in a Medicare Part D plan by placing a limit on what they will pay each year for their prescription drugs. The cap will be especially helpful for those who have high out-of-pocket medication costs and do not qualify for the federal Extra Help program.
After 2025, the Part D cap will increase each year. In 2026, the Part D cap will be $2,100.
Check out our guide
Get more details about how the Part D cap can help you, covered medications, and more with our guide to the Medicare Part D cap.
Medicare Prescription Payment Plan

The Medicare Prescription Payment Plan is a new voluntary Medicare Part D payment option going into effect on January 1, 2025. This program lets you spread your out-of-pocket drug payments throughout the calendar year but won’t lower them. You can opt in to the program through both traditional Medicare and Medicare Advantage Part D drug plans.
Anyone enrolled in a Part D plan who thinks they would benefit from the Medicare Prescription Payment Plan, regardless of their level of out-of-pocket spending, can opt-in to the program by contacting their plan. Information about the program is also on Medicare.gov and in your “Medicare & You” handbook.
Check out our guide
Is the Medicare Prescription Payment Plan right for you? Learn more about the plan, how and when to opt-in, how to estimate your monthly “smoothed” payments, and more details with our guide to the Medicare Prescription Payment Plan.
Other changes to the Medicare Part D Benefit
Several other important changes to the Medicare Part D program have been made since 2023:
- Elimination of the five percent coinsurance for Part D catastrophic coverage
- Expansion of the federal Extra Help program
- No cost-sharing for vaccines
- Insulin copay monthly cap
Elimination of the five percent coinsurance for Part D catastrophic coverage
As of January 1, 2024, people with Medicare Part D are no longer responsible for five percent prescription cost-sharing in the ‘catastrophic phase’ of coverage. This means that once a person reaches the catastrophic phase of coverage in 2024, they have no out-of-pocket responsibility for covered drugs for the remainder of the year.
With this change in effect, Part D enrollees who take only brand-name drugs in 2024 will have a cap of about $3,300 for calendar year 2024, according to a February 2024 Kaiser Family Foundation brief.
However, the Centers for Medicare and Medicaid (CMS) estimates that for some people enrolled in Medicare Part D who have very high drug costs, their out-of-pocket costs will be capped between $3,300 to $3,800.
This change in the Medicare Part D program ends December 31, 2024, and is replaced with the Medicare Part D cap of $2,000.
Expansion of the federal Extra Help program
The Low-Income Subsidy (LIS) or Extra Help program, is a federal program that helps people with limited income and assets pay for prescription medications and other related costs. To qualify for Extra Help, your income must be less than 150 percent of the federal poverty level.
Historically, there have been two versions of the program, the full program and a partial program. As of January 1, 2024, the partial program was eliminated. With full benefits, the majority, if not all, out-of-pocket costs for prescription medications will be covered.
Extra Help benefits
In 2025, people who qualify for Extra Help will pay:
- No plan deductible
- No premiums for Part D drug plans
- No more than $12.15 for each brand-name drug the plan covers, and $4.90 for generic medications.
How to apply
Historically, there have been two versions of the program, the full program and a partial program. As of January 1, 2024, the partial program was eliminated. With full benefits, the majority, if not all, out-of-pocket costs for prescription medications will be covered.
- Read PAN’s guide to the Extra Help program for details on eligibility and how to apply.
- Visit Medicare.gov to check your eligibility. From this page, you can follow their links to apply online through SSA.
- You can enroll in the Extra Help program by visiting SSA online directly.
- Call the SSA at 1-800-772-1213 to request a form SSA-1020 to apply for Extra Help.
- Visit ssa.gov/locator to get the telephone number for your local Social Security office.
- If you need help with your application, contact your State Health Insurance Assistance Program (SHIP) at ShipHelp.org or call 1-877-839-2675 to get the number for your local SHIP.

Vaccine full coverage
As of January 1, 2023, Medicare Part D plans and Medicare Advantage plans no longer require a deductible, coinsurance, or other cost-sharing requirements for adult vaccines that are recommended by the Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices. This includes the shingles vaccine.
Review the CDC’s list of adult vaccination insurance and payment for more information. Vaccines currently administered in doctors’ offices and paid for by Part B do not have cost-sharing obligations.
Insulin copay monthly cap of $35
As of January 1, 2023, cost-sharing for insulin products is limited to no more than $35 per month for people with Medicare insurance, including insulin covered under both Part D and Part B. Note: plans are not required to cover all brands and types of insulin. For a three-month supply of insulin, your costs can’t be more than $35 for each month’s supply of each covered insulin. This means you’ll generally pay no more than $105 for a three-month supply of covered insulin.
For insulin-related supplies (like syringes, needles, alcohol swabs, and gauze), you’ll pay 100 percent of the cost under Part B (unless you have Part D).
If you use a disposable insulin patch pump, you’ll continue to get your insulin through your Part D plan, and the insulin for your pump won’t cost more than $35 for a month’s supply of each covered insulin product.
If your Part D plan covers disposable insulin patch pumps, the pump is considered an insulin supply. Because it isn’t an insulin product, the pump isn’t subject to the $35 cap and might cost more than $35.
If you use an insulin pump that’s covered under Medicare Part B’s durable medical equipment benefit, or you get your covered insulin through a Medicare Advantage Plan, your insulin costs will be capped at $35 for a one-month supply. Learn more about Medicare insulin coverage.
Resources to learn more
- Visit your health plan’s website or call your plan for more information. Their phone number is on the back of your membership card.
- Visit Medicare.gov or call 1-800-MEDICARE (1-800-633-4227). TTY users: 1-877-486-2048.
- Visit the National Council on Aging for resources and information about Medicare.
- Contact your local State Health Insurance Assistance Program to receive free, personalized health insurance counseling.
- You can enroll in the Extra Help program through the Social Security Administration online at ssa.gov/ExtraHelp or by phone at 1-800-772-1213.
- Check your eligibility and learn more at PAN’s Extra Help education hub.
Watch our webinar: What you need to know about 2025 Medicare reforms
Download the webinar slides (pdf)
PAN Foundation financial assistance
Our grants
Even with the Medicare reforms that expand access and affordability, we know that many thousands of people will continue to face financial challenges in accessing their treatment. The PAN Foundation remains dedicated to providing financial assistance to people living with life-threatening, chronic, and rare diseases for their out-of-pocket treatment costs.
Additional resources
Grant amounts are changing based on disease fund, not insurance type. We’re considering all grant amounts and how what you need may change with the new Medicare reforms. If, for some reason, your PAN grant is not enough to cover your out-of-pocket costs, we offer some additional resources to help you:
- Additional funding: Patients, or their healthcare professionals, can apply for additional funding within the same initial 12-month grant eligibility period if they run out of funds and their grant balance is $0.
- FundFinder: You can use FundFinder to sign up for email or text message notifications to learn when financial assistance becomes available at any of the nine charitable patient assistance foundations.
This content was made possible in part by an educational grant from PhRMA.
Note: The PAN Foundation maintains full independence in the creation of educational content, ensuring that the materials produced are objective, evidence-based, and free from donor influence.
-
Subscribe to news
Sign up to receive PAN news, from helpful articles to action alerts.
Subscribe today -
-


